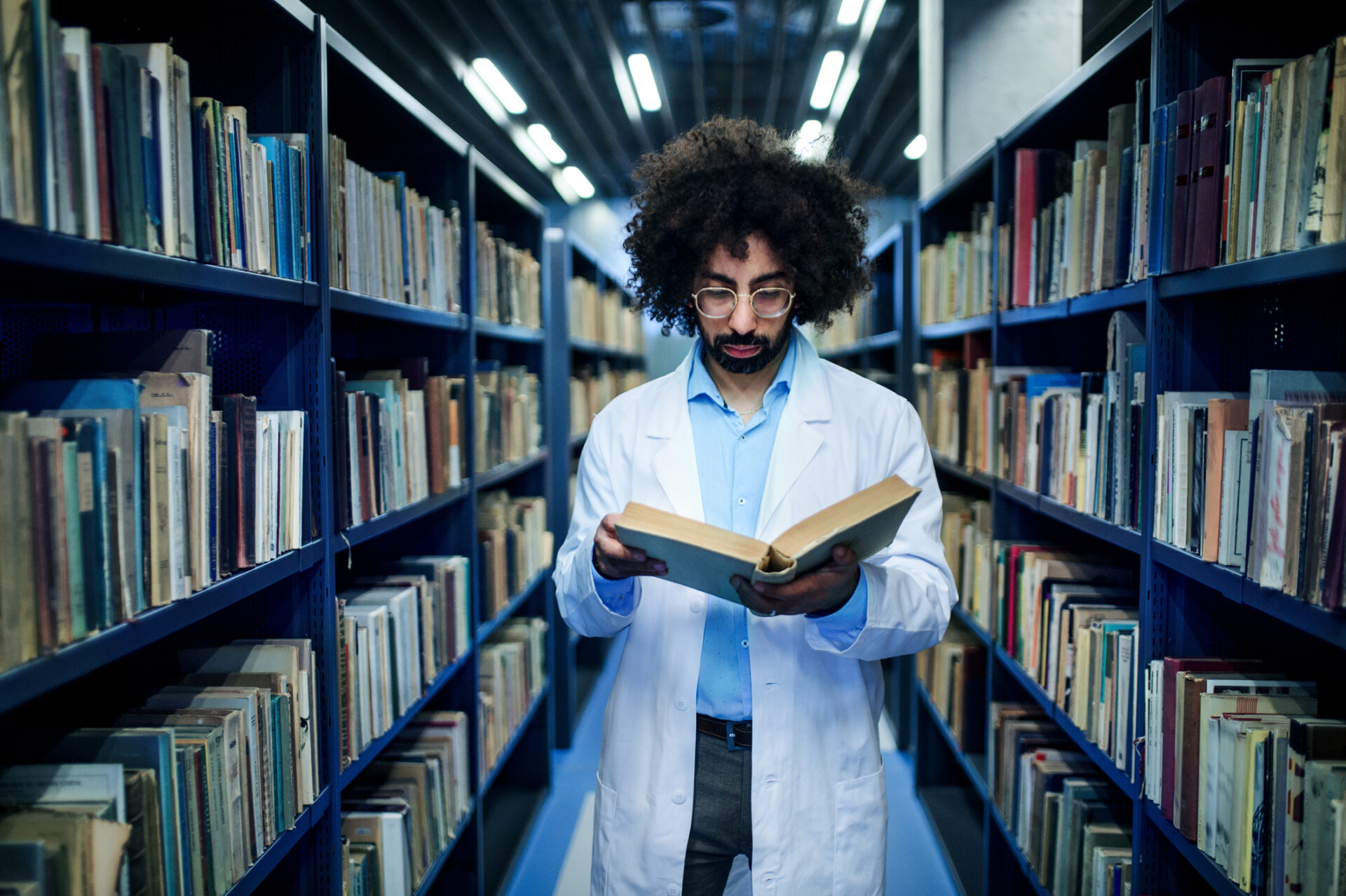
The profound changes in U.S. medical education in recent years have left schools balancing medical education costs, innovation and quality. Most Americans may not know that the USMLE Step 2 CS exam has been discontinued since the pandemic. This was the test that all medical students had to take to showcase their clinical skills. It tested on behaviors like bedside manner, empathy, and patient interactions.
Furthermore, the USMLE Step 1 exam underwent a critical transition, shifting from a scored to a pass-fail system. This is the exam that tests medical students’ ability to integrate their knowledge of the essential basic sciences in a clinical setting.
The former Step 2 CS exam posed a substantial challenge, particularly for international students, due to its steep cost and the logistical demands of travel. Advocates for the Step 1 change argued the pressures of needing a high score posed unnecessary added stress on medical students. However, the alteration of the Step 1 exam’s scoring system marks a significant deviation from its previous role. Historically, this score was sited as the most important factor for residency program directors in selecting candidates. Its transition to a pass/fail system indicates a paradigm shift in the residency selection process moving forward.
The COVID-19 pandemic accelerated some changes and, in many ways, challenged traditional educational models. It propelled many institutions to invest in providing wider access to virtual curriculum options. It brought into question the correlation between standardized testing performance and actual clinical proficiency. While these changes were partly necessitated by practical constraints, they also reflected a growing recognition that physician competence encompasses a lot more than test scores.
Medical Education Costs, Innovation and Quality: Finding Balance
As medical education costs continue to rise, there’s an urgent need to balance educational innovation with the maintenance of high standards. The traditional model of medical education which has been slow to evolve, must adapt to a rapidly changing healthcare environment without compromising on the quality of training.
One key metric to consider is patient satisfaction, which is crucial for healthcare quality. A study published in the “Journal of the American Medical Association” found that effective communication and empathy–skills emphasized in clinical training–are directly linked to higher patient satisfaction levels. This suggests that while changes in testing procedures are notable, the core of medical education, which fosters these essential skills, remains critical.
The Future: Innovation with Integrity
The shift in medical education standards should not be viewed merely as a reduction in rigor but as an opportunity for innovation. For instance, virtual clinical experiences and telehealth training, as offered by AMOpportunities, provide a flexible, cost-effective, and safe alternative to traditional models, reflecting the future of medical practice. These programs offer a diverse and rich learning environment that prepares students for the evolving demands of healthcare.
The changes in medical education, driven by necessity and innovation, should not be seen as a lowering of standards but as an evolution. The challenge lies in balancing these innovations with the maintenance of high-quality training. As the landscape of healthcare continues to shift, it is imperative that medical education adapts, ensuring that the doctors of tomorrow are equipped not only with the knowledge but also with the empathy, communication skills, and practical experience to provide the best care to a diverse range of patients. As we move forward, it is essential to continuously evaluate and refine these educational models to ensure they meet the needs of both trainees and patients in a rapidly changing world.





Leave A Comment